RESEARCH ARTICLE |
https://doi.org/10.5005/jp-journals-10016-1300 |
Fetomaternal Complications of In Vitro Fertilization Pregnancies in a Tertiary Center
1-3Department of Obstetrics and Gynaecology (OBG), Ramaiah Medical College and Hospitals, Bengaluru, Karnataka, India
Corresponding Author: Vanshika Balani, Department of Obstetrics and Gynaecology (OBG), Ramaiah Medical College and Hospitals, Bengaluru, Karnataka, India, Phone: +91 9148641380, e-mail: vanshika.balani@gmail.com
Received on: 22 October 2022; Accepted on: 23 November 2022; Published on: 28 December 2022
ABSTRACT
Introduction: Over the past decade, the use of assisted reproductive technology (ART) has increased dramatically. In vitro fertilization (IVF) is the most frequently practiced ART procedure. There has been an increasing trend in a number of pregnancies in IVF conception since it was first introduced in 1981. Multifetal gestation and its outcomes are the greatest risks of IVF pregnancy. There is an increased risk of prelabor rupture of membranes (PROM), preterm labor, low birth weight (LBW), and small for gestational age infants. It is also associated with increased maternal complications during pregnancy, including gestational diabetes mellitus (GDM), preeclampsia, intrahepatic cholestasis of pregnancy, placental abruption, placenta praevia, adherent placenta, polyhydramnios, and postpartum hemorrhage. Thus, pregnancies after IVF conception require more vigilant monitoring.
Objective: Assess maternal and fetal complications of IVF pregnancies and IVF conception.
Study design: Retrospective single-arm analysis of pregnancies with IVF complications over a period of 3 years from September 2014 to August 2017.
Results: A total of 104 women underwent IVF conception, with the highest incidence in women of age more than 30 years (56.73% of the cases). There were eight cases of abortion. Among the total cases who underwent IVF conception, 73 (70%) women were primigravidae, and 31 (30%) were multigravidae. The risk of maternal complications was 87.5%. Multifetal gestation was the most common maternal complication (39.4%), with an incidence of twin pregnancy of 37.5%, out of which 32.7% were dichorionic diamniotic (DCDA) twins and 4.8% were monochorionic diamniotic (MCDA) twins, followed by preterm labor (17.3%). The total number of viable newborns delivered was 140, with 43.2% being LBW (<2.5 kg). A total of 45 babies (32.1%) required neonatal intensive care unit (NICU) admissions, out of which three babies (2.1%) succumbed.
Conclusion: There is a need for more vigilant monitoring of IVF pregnancies in view of a higher rate of maternal and fetal complications.
How to cite this article: Seshadri JG, Balani V, Kempaiah SB. Fetomaternal Complications of In Vitro Fertilization Pregnancies in a Tertiary Center. Int J Infertil Fetal Med 2022;13(3):116-120.
Source of support: Nil
Conflict of interest: None
Keywords: Dichorionic diamniotic, In vitro fertilization, Low birth weight, Monochorionic diamniotic, Neonatal intensive care unit, Pulmonary embolisms.
INTRODUCTION
Infertility is an immensely growing public health and social problem. IVF-embryo transfer (ET) has become an increasingly used treatment for infertile patients.1 Large meta-analysis studies have demonstrated adverse maternal and neonatal outcomes associated with ART procedures in spite of the advancements in various treatment protocols and freezing techniques. The epigenetic changes related to treatment along with the altered implantation process involved in IVF with suboptimal placentation could be the cause for the same.2 Whether the pregnancy is a singleton or multiple gestations determines the sole important determinant for their outcomes.3 Many women who undergo IVF are older and hence more likely to have pregnancy complications, so advanced maternal age is considered an important factor.
Singleton pregnancies after IVF are associated with an increased rate of complications, unlike the multifetal gestations achieved by IVF, which have similar outcomes to those of multiple gestations conceived spontaneously.4,5 This factor is due to the high proportion of singletons that result from vanishing twins or triplets.6
Women with IVF-conceived singleton pregnancies are at increased risk of gestational diabetes, preeclampsia, placenta praevia, and perinatal mortality.7 Many studies also report increased neonatal morbidity due to prematurity and LBW in children born to women with IVF pregnancies. Babies born by ART also have a higher risk of NICU admissions. These admissions are mostly for supportive care to initiate feeding or due to prematurity. However, it is seen that the long-term developmental outcomes in children conceived by IVF have been reassuring and the majority develop normally.
Hence looking into all the complications of IVF pregnancies, the objective of our paper was to assess these complications and the risks they pose in society.
OBJECTIVE
To assess fetomaternal complications of IVF pregnancies in a tertiary center.
MATERIALS AND METHODS
This is a retrospective study of antenatal cases with IVF conception in the Department of Obstetrics and Gynaecology of Ramaiah Medical College, Bengaluru over a period of 3 years.
Statistical Analysis
-
Descriptive statistics were analyzed with Statistical Package for Social Sciences version 17.0 software. Continuous variables were presented as mean ± standard deviation. Categorical variables were expressed as frequencies and percentages.
-
Pearson’s chi-squared test or the chi-square test of association was used to determine whether there was a relationship between two categorical variables.
-
p < 0.05 was considered to be statistically significant.
RESULTS
The age profile of the patients varied from 24 to 40 years. As shown in Figure 1, there were 73 patients whose ages ranged from 26 to 35 years.

Fig. 1: Age groups of the women who underwent IVF conception
There were 72 (69.2%) cases of primary infertility, whereas 32 (30.8%) cases were of secondary infertility. The most common positive past history was polycystic ovarian disease, seen in 6.7% of patients.
Outcomes of Pregnancy
Of the 104 pregnancies in the study, eight resulted in abortion (7.7%) and 48 resulted in preterm birth (46.1%).
There were eight cases of abortion, of which five were spontaneous abortions and three were induced; two were because of congenital anomalies, and one was due to abnormal Doppler, which was identified on sonography. There were three cases of second-trimester pregnancy loss, one due to vasa praevia with preterm labor, another due to abruption placenta, and the third being idiopathic.
Complications in pregnancy are enlisted in Table 1 with the comparison of the rate of complications in single and multiple pregnancies. Multiple gestations were seen in 41 cases (39.4%) of which 39 (37.5%) cases were of twins and 2 (1.9%) cases of triplets. Among twin gestations, 34 (32.7%) were DCDA twins and 5 (4.8%) were MCDA twins. Around 21 patients in the study developed hypertensive diseases of pregnancy (20.2%), of whom 10 patients developed preeclampsia; 10 patients developed gestational diabetes mellitus, 9.6% each. Cases with multiple pregnancies had a higher rate of preterm labor (34.1%) and hypertension-complicating pregnancies (31.7%).
| Complication | Frequency | Percentage | |||||
|---|---|---|---|---|---|---|---|
| Singleton pregnancies (n = 63) | Multiple gestations (n = 41) | Total (n = 104) | Singleton pregnancies | Multiple gestations | Total | ||
| Abortion | 3 | 5 | 8 | 4.8 | 12.2 | 7.7 | |
| Preterm labor | 4 | 14 | 18 | 6.3 | 34.1 | 17.3 | |
| Preterm premature rupture of membranes (PPROM) | 7 | 6 | 13 | 11.1 | 14.6 | 12.5 | |
| Hypothyroidism | 17 | 7 | 24 | 27 | 17.1 | 23.1 | |
| Gestational diabetes mellitus (GDM) | 8 | 2 | 10 | 12.7 | 4.9 | 9.6 | |
| Hypertension complicating pregnancy | Total | 13 | 8 | 21 | 20.6 | 31.7 | 20.2 |
| Preeclampsia | 4 | 6 | 10 | 6.3 | 14.6 | 9.6 | |
| Hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome | 1 | 0 | 1 | 1.6 | 0 | 1 | |
| Anemia | 3 | 4 | 7 | 4.8 | 9.7 | 6.7 | |
| Intrauterine growth restriction (IUGR) | 3 | 2 | 5 | 4.8 | 4.9 | 4.8 | |
| Antepartum hemorrhage | 1 | 2 | 3 | 1.6 | 4.9 | 2.9 | |
| Oligoamnios | 2 | 2 | 4 | 3.2 | 4.9 | 3.8 | |
| Polyhydramnios | 1 | 0 | 1 | 1.6 | 0 | 1 | |
| Acute fatty liver of pregnancy (AFLP) | 1 | 0 | 1 | 1.6 | 0 | 1 | |
| Jaundice in pregnancy | 0 | 1 | 1 | 0 | 2.4 | 1 | |
| Thrombocytopenia of pregnancy | 1 | 0 | 1 | 1.6 | 0 | 1 | |
The age groups of women in the study ranged from 24 to 44 years of age. Table 2 compares the frequency of complications in various age groups. Women over 35 years of age had a higher incidence of hypertension-complicating pregnancy and fetal growth restriction.
| Complication | <35 years | Percentage (n = 78) | 35–40 years | Percentage (n = 20) | >40 years | Percentage (n = 6) | |
|---|---|---|---|---|---|---|---|
| Abortion | 2 | 2.6 | 4 | 20 | 2 | 33.3 | |
| Multiple pregnancy | Total | 33 | 42.3 | 8 | 40 | 0 | 0 |
| Twins | 31 | 39.7 | 8 | 40 | 0 | 0 | |
| Triplets | 2 | 2.6 | 0 | 0 | 0 | 0 | |
| Preterm labor | 35 | 44.9 | 11 | 55 | 2 | 33.3 | |
| Preterm premature rupture of membranes (PPROM) | 9 | 11.5 | 2 | 10 | 2 | 33.3 | |
| Hypothyroidism | 17 | 21.8 | 6 | 30 | 1 | 16.7 | |
| Gestational diabetes mellitus (GDM) | 7 | 9 | 2 | 10 | 1 | 16.7 | |
| Hypertension complicating pregnancy | Total | 12 | 15.4 | 8 | 40 | 1 | 16.7 |
| Preeclampsia | 3 | 3.8 | 6 | 30 | 1 | 16.7 | |
| Hemolysis, elevated liver enzymes, low platelet count (HELLP) syndrome | 1 | 1.3 | 0 | 0 | 0 | 0 | |
| Anemia | 6 | 7.7 | 1 | 5 | 0 | 0 | |
| Intrauterine growth restriction (IUGR) | 2 | 2.6 | 2 | 10 | 1 | 16.7 | |
| Antepartum hemorrhage | 3 | 3.8 | 0 | 0 | 0 | 0 | |
| Oligoamnios | 2 | 2.6 | 1 | 5 | 1 | 16.7 | |
| Polyhydramnios | 0 | 0 | 0 | 0 | 1 | 16.7 | |
| Acute fatty liver of pregnancy (AFLP) | 1 | 1.3 | 0 | 0 | 0 | 0 | |
| Jaundice in pregnancy | 1 | 1.3 | 0 | 0 | 0 | 0 | |
| Thrombocytopenia of pregnancy | 1 | 1.3 | 0 | 0 | 0 | 0 | |
Table 3 shows the mode of delivery in patients who underwent IVF pregnancy. Around 67.3% of cases underwent a cesarean section, the most common indication being maternal choice (34.3%), followed by twin gestation in 10% and abnormal presentation in 10% of cases.
| Mode of delivery | Frequency | % | |
|---|---|---|---|
| Lower segment Cesarean section (LSCS) | Total | 70 | 67.3% |
| Elective | 20/70 | 28.6% | |
| Emergency | 50/70 | 71.4% | |
| Premature triple-vessel disease (PTVD) | Total cases | 15 | 14.4% |
| Forceps-assisted PTVD | 3/15 | 20.0% | |
| Full-term vaginal delivery (FTVD) | Total cases | 7 | 6.7% |
| Forceps-assisted FTVD | 1/7 | 14.3% | |
| Vac FTVD | 3/7 | 42.9% |
A total of 140 babies were born to the study group cases with a mean birth weight of 1.76 kg. Figure 2 shows the birth weight of the 140 babies. Around 48.5% of neonates weighed <2 kg, most of these cases being of multiple gestations. Neonates with LBW were seen in only six cases of singleton gestation. LBW of babies was primarily due to prematurity with a p-value of <0.001.
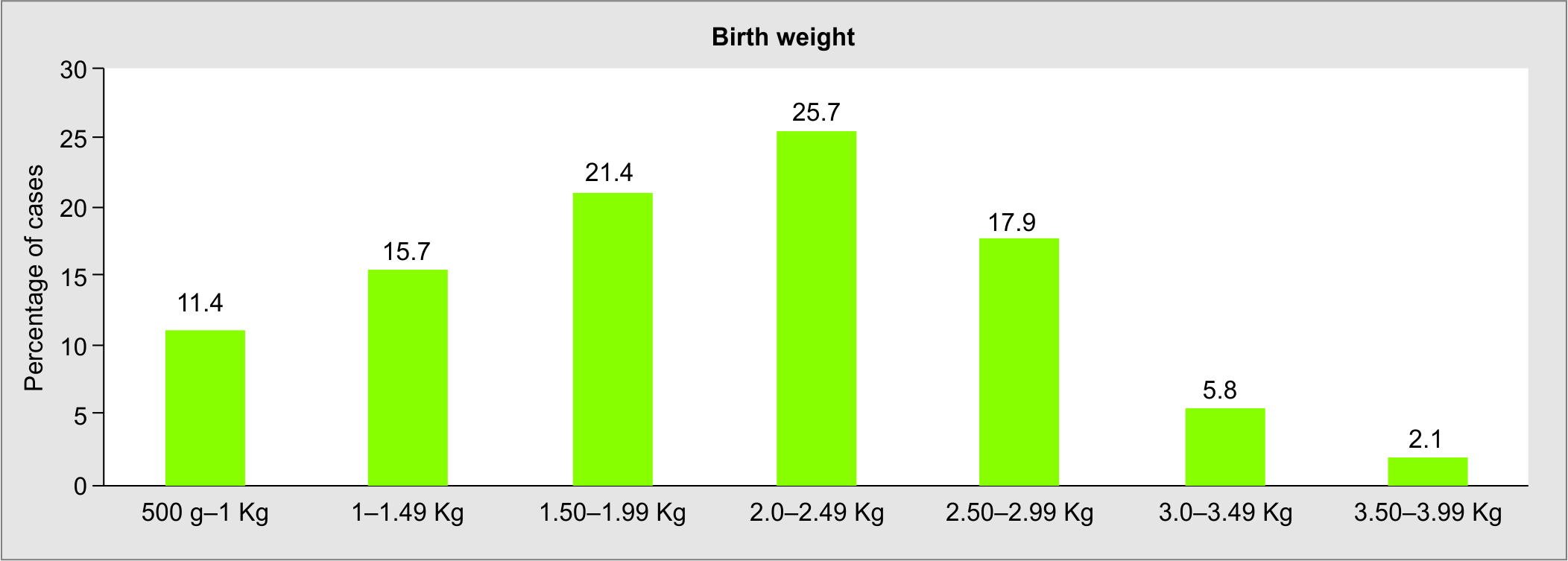
Fig. 2: Histogram showing birth weight of newborns in IVF pregnancies
Among 140 of neonates, 45 babies (32.1%) required NICU admission. The most common cause of NICU admission was prematurity and complications related to it (22.1%), followed by respiratory distress syndrome, seen in 4.2% of the neonates. There were two cases of intrauterine fetal demises noted, one in a case of monochorionic monoamniotic twins with twin-to-twin transfusion and one in a term singleton pregnancy with GDM. There were three neonatal deaths in the study, the first due to cardiac anomaly patent ductus arteriosus in a preterm baby, the second in a case of DCDA twins with preterm birth due to periventricular leukomalacia, and the third in a case with severe preeclampsia due to respiratory distress syndrome.
DISCUSSION
This study shows the increased risks of pregnancy complications, perinatal complications, and poor neonatal outcomes related to ART.
Table 4 compares the rates of complications in pregnancies with IVF conception in the present study with those in studies by Kathpalia et al. and Gui J et al.8,9
| Complications | Present study | Kathpalia et al. | Gui et al. |
|---|---|---|---|
| Gestational hypertension | 20.2 | 8.5 | 9.4 |
| Preeclampsia | 9.6 | 4.6 | 3.7 |
| Gestational diabetes mellitus (GDM) | 9.6 | 3.6 | 11.7 |
| Intrahepatic cholestasis of pregnancy | 1 | - | 11.4 |
| Multiple gestations | 39.4 | 27.6 | 37.1 |
| Preterm labor | 17.3 | 21.5 | 38.8 |
| Preterm premature rupture of membranes (PPROM) | 12.5 | 3.8 | 9.8 |
| Antepartum hemorrhage (APH) | 2.9 | 2.2 | 8.5 |
| Oligohydramnios | 3.8 | 0.7 | 4.8 |
| Polyhydramnios | 1 | 0.7 | 2.3 |
Studies indicate that patients who underwent IVF were more likely to develop gestational hypertension, preeclampsia, GDM, intrahepatic cholestasis of pregnancy, placental abruption, and placenta praevia than spontaneously conceived pregnancies.7,10 This may be due to parental characteristics, underlying medical conditions associated with subfertility and infertility, the use of ovulation induction medications, and conditions during embryo preparation.7
The most common medical comorbidity observed in the study was hypertension complicating pregnancy. Several risk factors have been identified for the increased incidence of hypertensive disorder in IVF pregnancies, like obesity, advanced maternal age, polycystic ovarian syndrome (PCOS), multiple gestations, systemic lupus erythematosus, diabetes, and pregestational hypertension.9 Many of these are common in infertile patients undergoing IVF. Other contributing factors could be endometrial dysplasia following ovarian stimulating hormone treatment, which results in deficient trophoblastic invasion and defective placentation.9,10 In IVF pregnancies, the endometrial environment is affected by altered hormone levels, which may disturb the development of the maternal-fetal interface, leading to deficient placental function.10 Thus, abnormalities in the placental vascular system are more common in women with IVF pregnancies. GDM was seen in 9.6% of patients. The increased rates of GDM may be due to the higher incidence of PCOS in infertile patients. Pregnancy-induced insulin resistance superimposes on the physiologic insulin resistance in PCOS women.11
A large percentage of the study population underwent lower segment Cesarean section (LSCS), the most common indication being a maternal choice, in 34.3% cases. This represents the anxiety and apprehension among these women, which may also contribute to prematurity. It may also be that women with pregnancies resulting from IVF and their physicians select cesarean delivery because of the greater investment of time and money in achieving pregnancy; and that physicians prefer to ensure an optimal outcome by recommending elective cesarean delivery or proceed with cesarean delivery at the first hint of any problem during labor.12
Even term infants in IVF pregnancies were at a higher risk of LBW, with 30.5% of term babies being LBW.
Table 5 compares the incidence of Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) score <7 at 1–5 minutes; in the present study, 36.5% of babies had an APGAR score of <7 at 1 minute and 6.7% had an APGAR score of <7 at 5 minutes. These results were comparable to the study by Kathpalia et al.8
| Present study | Kathpalia et al. | Gui et al. | |
|---|---|---|---|
| Low birth weight (LBW) babies | 43.2 | 30 | 36.5 |
| 1 minute Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) ≤7 | 36.5 | 32 | 5 |
| 5 minute APGAR ≤7 | 6.7 | 5 | 0.9 |
It was difficult to eliminate potential confounding factors because of the retrospective design of our study and also because of the study being conducted at a single tertiary center. The number of patients in the study was relatively less in number. There was no data collected on the specific cause of infertility, baseline hormone levels, ovarian stimulation protocol used, and the number and quality of embryos transferred. Thus, the effect of these factors on maternal and neonatal outcomes cannot be inferred.
CONCLUSION
A total of 104 cases were enrolled for the study. Being a retrospective observational study, there were no controls. Hence the findings obtained were compared with those available in the literature. The commonest complications included multiple pregnancies and hypertension complicating pregnancy, and these complications observed were sequelae of twin gestation. These patients should be treated as high-risk cases and monitored vigilantly.
There is a need to do further multicentric studies along with the controls to compare the results with pregnancies conceived spontaneously.
ORCID
Jyothi G Seshadri https://orcid.org/0000-0001-9947-9450
Vanshika Balani https://orcid.org/0000-0002-3455-906X
REFERENCES
1. Wang YA, Sullivan EA, Black D, et al. Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertil Steril 2005;83(6):1650–1658. DOI: 10.1016/j.fertnstert.2004.12.033
2. Ganer Herman H, Mizrachi Y, Shevach Alon A, et al. Obstetric and perinatal outcomes of in vitro fertilization and natural pregnancies in the same mother. Fertil Steril 2021;115(4):940–946. DOI: 10.1016/j.fertnstert.2020.10.060
3. Vulliemoz NR, McVeigh E, Kurinczuk J. In vitro fertilisation: perinatal risks and early childhood outcomes. Hum Fertil (Camb) 2012;15(2):62–68. DOI: 10.3109/14647273.2012.663571
4. ACOG COMMITTEE OPINION Number 671 · September 2016 Committee on Obstetric Practice Committee on Genetic
5. Schieve LA, Meikle SF, Ferre C, et al. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med 2002;346(10):731–737. DOI: 10.1056/NEJMoa010806
6. Pandey S, Shetty A, Hamilton M, et al. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update 2012;18(5):485–503. DOI: 10.1093/humupd/dms018
7. Chasen ST, Luo G, Perni SC, et al. Are in vitro fertilization pregnancies with early spontaneous reduction high risk? Am J Obstet Gynecol 2006;195(3):814–817. DOI: 10.1016/j.ajog.2006.06.022
8. Kathpalia SK, Kapoor K, Sharma A. Complications in pregnancies after in vitro fertilization and embryo transfer. Med J Armed Forces India 2016;72(3):211–214. DOI: 10.1016/j.mjafi.2015.11.010
9. Gui J, Ling Z, Hou X, et al. In vitro fertilization is associated with the onset and progression of preeclampsia. Placenta 2020;89:50–57. DOI: 10.1016/j.placenta.2019.09.011
10. Bartsch E, Medcalf KE, Park AL, et al. Clinical risk factors for pre-eclampsia determined in early pregnancy: systematic review and meta-analysis of large cohort studies. BMJ 2016;353:i1753. DOI: 10.1136/BMJ.i1753
11. Szymanska M, Horosz E, Szymusik I, et al. Gestational diabetes in IVF and spontaneous pregnancies. Neuro Endocrinol Lett 2011;32(6):885–888. PMID: 22286793.
12. Rebar RW Why are cesarean delivery rates higher with IVF pregnancies? OB/GYN Clinical Alert 2018.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.